While many people have heard of the sciatic nerve and sciatica, it is rare to hear people talk about the pudendal nerve, or understand how unwanted pelvic symptoms may be connected to issues with that nerve. Yet, many pelvic floor problems are affected by the function or dysfunction of the pudendal nerve, and understanding the anatomy and the roles it plays in our body could unlock the key to healing.
The pudendal nerve is the primary nerve in the pelvis, named after the Latin word pudendum, which translates to “parts to be ashamed of”. Given the etymology, it is not a surprise that the pudendal nerve is hardly talked about. However, the pudendal nerve is a major nerve in our bodies and responsible for integral functions of life – namely your ability to control when you pee and poop, and your ability to engage in and enjoy sexual intimacy. Understanding the anatomy, function, and symptoms associated with an irritated pudendal nerve may help people better understand their own bodies, identify and seek treatment when things do not feel right, and find the right approach to pelvic healing.
Anatomy and Function
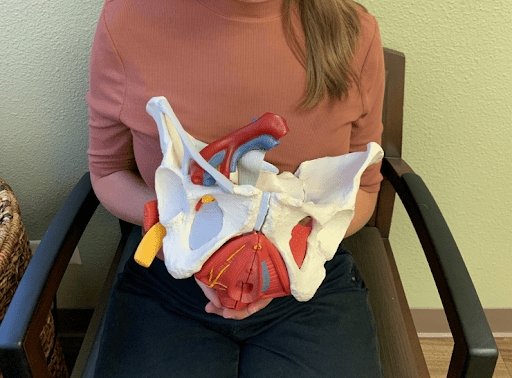
The pudendal nerve is responsible for supplying sensation to the genitals, perineum (area between the vulva and anus or testicles and anus), and anal region, as well as controlling the majority of pelvic floor muscles. Each person has a paired right and left nerve that originates from a bundle of nerves near the lower segments of the tailbone, known as the sacrum. The pudendal nerve forms from the nerve roots on segments 2, 3, and 4 of the sacrum and then winds around the pelvis, traveling through the upper buttock region, and with the sciatic nerve through an opening in the back of the pelvis known as the greater sciatic foramen. It then exits through another opening called the lesser sciatic foramen. After that, the nerve runs alongside a vein and artery through a narrow passageway known as Alcock’s canal or the pudendal canal. The pudendal nerve then divides into three branches.
The three branches of the pudendal nerve (from back to front) include the inferior rectal nerve, the perineal nerve, and the dorsal nerve. The inferior rectal nerve carries information about sensation from around the anal sphincter and controls the anal sphincter muscles. The perineal branch is responsible for sensation to the area between the vulva and anus or testes and anus, and controls the urethral sphincter muscles. Lastly, the dorsal nerve sends sensory information from the penis or clitoris and plays an important role in sexual arousal and sexual function.
Pudendal Nerve Entrapment & Pudendal Neuralgia
If there is injury or irritation to the pudendal nerve, people may experience pain in the areas supplied by any or all of the three branches, or issues with controlling bladder, bowel, and sexual function.
Pudendal nerve injury can result from accidents or traumatic injuries, surgical complications, difficulty with labor and delivery, tumors, from diabetes-related nerve problems, or more commonly from prolonged compression such as in cycling, prolonged sitting, or repetitive movements putting pressure on the nerve. Prolonged compression on the nerve, called pudendal nerve entrapment syndrome, can cause pudendal neuralgia, a very painful and often debilitating condition. People who suffer from pudendal neuralgia may experience stabbing, burning, itching, or electric-like pain around the anus, perineum, or genitals.
Pain that increases with sitting is often a hallmark sign that the problem might be coming from the pudendal nerve. The pudendal nerve is commonly entrapped at certain points along its path through the pelvis, including around the piriformis muscle, between two strong sacral ligaments, at the Alcock’s canal, or at terminal branches.
Treatment for Pudendal Neuralgia
Treatment for pudendal neuralgia may involve multiple approaches. Often conservative management with teaching behavioral and lifestyle modifications and physical therapy can make tremendous improvements or resolve symptoms entirely.
Given that pudendal neuralgia has to wind through the pelvis, pelvic health physical therapy can help to identify areas where the nerve may be compressed and treat those areas accordingly. For example, if the nerve is compressed at the piriformis muscle, your pelvic health physical therapist can help release, stretch, and retrain that muscle to decrease irritation on the nerve. Treatment may also include helping you reduce tension-holding patterns in your pelvic floor muscles, or improve movement strategies that put pressure on the nerve, as well as teaching modifications to eradicate symptoms or decrease the frequency and intensity of symptom flare-ups.
Aside from physical therapy, other treatments for pudendal neuralgia include cognitive behavioral therapy for chronic pain, which can be a powerful adjunct treatment to reduce and/or alleviate symptoms. Pharmacological therapy may include medications such as amitriptyline, duloxetine, or gabapentin among others. Medical procedures such as nerve blocks administered with image guidance can reduce symptoms temporarily and may be repeated regularly for relief. Surgical decompression by removing some nerve fibers and reducing compression of the nerve has been shown to provide many with effective long-term treatment for pudendal nerve entrapment as well. Nerve stimulators and pulsed radiofrequency ablation may also help people manage symptoms, and are often the last resort when people have been unable to find relief from all other treatments.
Final Thoughts
Pudendal neuralgia is often missed or misdiagnosed by healthcare providers, and many people unsuccessfully spend time and resources on getting treatment for other conditions before receiving an appropriate diagnosis of pudendal neuralgia. Chronic pelvic pain, such as that with undiagnosed pudendal neuralgia, can present financial and mental health burdens, and is even associated with higher levels of depression.
Though pudendal nerve entrapment and pudendal neuralgia can significantly impact quality of life, it is important to note that there are treatment options available. Primary treatment options include conservative management with physical therapy and lifestyle modifications, and also may include behavioral therapy, pharmacology treatments, and medical procedures. For further information on pudendal neuralgia and physical therapy treatment options, contact N2 today or reach out to your local pelvic health physical therapist.
Sources:
https://www.ncbi.nlm.nih.gov/books/NBK544272/
https://www.etymonline.com/word/pudendum
https://pubmed.ncbi.nlm.nih.gov/25828522/
The Tools of Pelvic Floor Physical Therapy
https://n2physicaltherapy.com/b/the-tools-of-pelvic-floor-physical-therapy